Living with Ulcerative Colitis
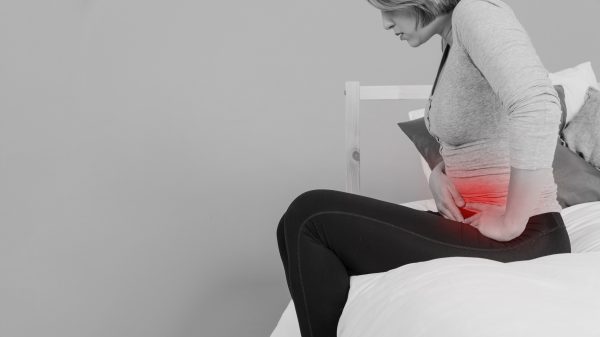
Today, May 19, is World IBD Day. For the first 20 years of my life, I lived blissfully unaware of the inflammatory bowel disease (IBD), ulcerative colitis (UC). Sure, I’d heard of stomach upset, suffered through childhood digestive woes and stomach viruses, but I didn’t know there was anything more than the ever-fleeting “nervous stomach” term I’d been assigned as a kid. Those first days of school tummy jitters, the clamminess before big tests or speaking in front of the class, the waves of nausea after making an ass of myself in front of my crush, etc.
I took an acid-reducing medicine while in 11th grade and the occasional half-tablet of Imodium-AD to settle my digestive system, but it wasn’t until college that I started having severe problems.
The changes were subtle at first, so subtle that I only recognize them now as I reflect on that time in my life.
Pre-Diagnosis
Change #1: Fatigue

Even though I thought I should be young and vibrant at 20 years old, I was exhausted all the time. I got to the point where I would sleep a lot during my days off work. I thought it was just because I was experiencing some personal drama. Because I had just moved into my own apartment, no one knew how much I slept.
Change #2: Nausea
In the mornings, especially, I was queasy to the point of not wanting to eat. I wasn’t pregnant and could find no other explanation except for needing acid reducing medicine again, so I started taking it.
Change #3: Weight loss

The weight loss was slow at first. I had lost weight rather than gain the dreaded “freshman 15” upon starting college. Several pounds due to the increased amount of exercise I was getting walking all over campus. My jeans from high school were soon too large. I bought smaller sizes until there were no smaller sizes.
Change # 4: Unusual bowel symptoms

Problems I attributed to eating fast food and unhealthy foods from the cafeteria were something more. At times, I would have to run to make it to the restroom in time, which was embarrassing.
Change #5: The eye-opener. Blood.
After discovering blood in the bathroom when I wasn’t on my period, I went to see a doctor.
Doctor’s visit
The doctor put me on a fiber treatment regimen, which made everything worse. I got sicker and sicker. Weaker and weaker. The bloody stool continued. At that point, I was referred to a gastroenterologist for a series of tests because one of the possibilities was colon cancer.
Colonoscopy
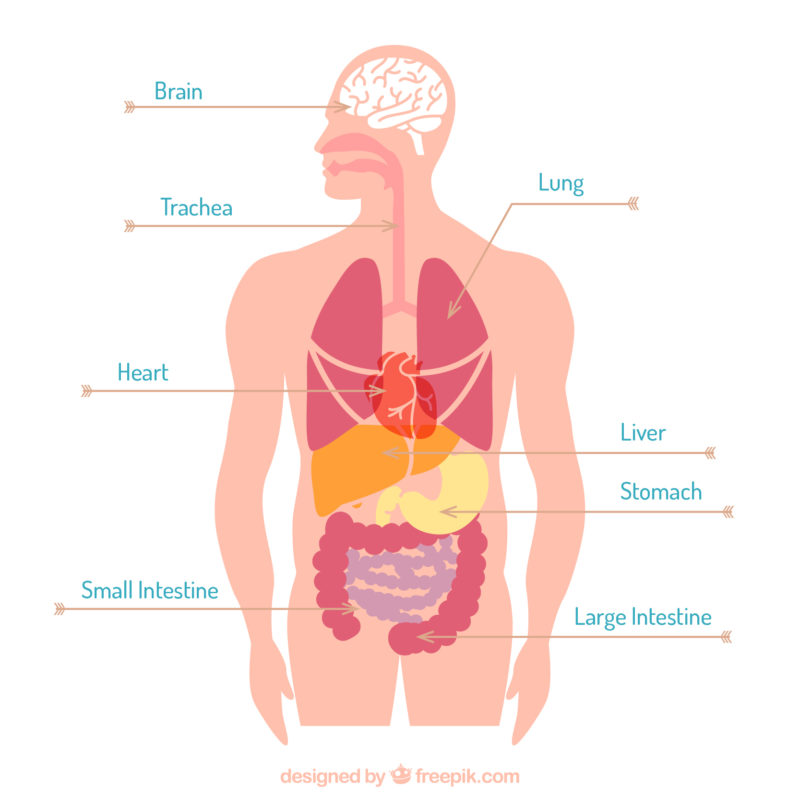
The test itself wasn’t bad thanks to the happy juice you get at the hospital. The prep-work for the test when I was already so sick was living hell. To be frank, a colonoscopy is an inside look at your colon and large intestine. For this test, your bowels must be empty. The prep-work is a day of emptying them with the help of medication.
Diagnosis
I didn’t have colon cancer. I had moderate left-sided ulcerative colitis. My large intestine, mostly on the left side, was inflamed and infiltrated by bleeding ulcers. There are many treatments, but the only cure is removal of the colon. Like cancer, UC goes through periods of being active or being in remission. Remission (no major symptoms) is always the goal.
Medication trials
I chose medication therapy under the direction of the specialist. It took seven different types of medication before I found the combination that worked for me. I won’t bore you with all the details of the medications, but there is a reason so many drugs exist: because everyone’s body reacts differently.

While trying to get the medications right, I was in active flare-ups, one right after the other. I couldn’t keep food in my digestive system long enough for my body to absorb the nutrients. My hair thinned, I had dark circles under my eyes, my gums bled from all the vomiting. I missed a lot of work and forced myself to be there on the days that I showed up. I was dependent on (doctor-prescribed) steroids to keep the flare-ups under control, but each time I would taper off, the flare would start back even worse.
Hospitalization
My mom knew I was sick, but she didn’t know how bad until she got to my apartment, and I asked her to take me to the hospital.

After a week in the hospital, more tests, IV nutrition, and new medication, I was released to my mother’s care. I still wasn’t well. I didn’t know how to eat. It sounds crazy to be 21 years old and not be able to eat, but I couldn’t. I would gag and vomit when any measurable amount of solid food hit my stomach. I stayed at my parents’ home that week, and I know they were frustrated with me. They might have thought my inability to eat was something psychological as though I were suffering from an eating disorder, but it wasn’t the case. My stomach had shrunk, and my esophagus would spasm. I thought I was going to die.

After that week of new medication and forcing myself to eat a bowl of dry cereal (one piece at a time) throughout the day, my mom took me back to my apartment. I didn’t know what to do with myself. I discovered I could eat bland things like plain turkey sandwiches and animal crackers.
Rebuilding my life
UC meant having a name for the pain for the first time. A name for the reason I felt like shit all the time (no pun intended). Two of the medications I started after my hospitalization I still take now, 16 years later. One of them is a chemotherapy pill that requires me to undergo liver tests every year to monitor for signs of liver failure. My dosage is low, and my liver is tolerating the medication.
I’ve been blessed. In 16 years, I’ve had only three flares that required a course of steroids (six-eight weeks of a slowly tapering dosage). Steroids are amazing, but the side effects are hard to deal with. Some of the more noticeable ones for me were weight gain, night sweats, and insomnia.
My UC went into remission during both pregnancies. I continued my medication throughout each under close watch from my gastroenterologist and OB. I had to give up my hopes for breastfeeding, but it was just as important to keep me healthy for my babies, and stopping my meds wasn’t an option.
But you don’t look sick?
 Yeah, that’s why UC is often referred to as an invisible disease. Even in official remission, UC is with me every day. I smile even when I don’t feel well. I am often tired, though I get plenty of sleep now. I always have dark circles under my eyes. I worry that any digestive discomfort could be the start of a flare. Catching a severe stomach virus could land me in the hospital if I were unable to take my meds. I can’t ever forget my meds. Though I try not to let it rule my life, the fear is always there that I will develop colon cancer since IBD patients are more likely to develop it.
Yeah, that’s why UC is often referred to as an invisible disease. Even in official remission, UC is with me every day. I smile even when I don’t feel well. I am often tired, though I get plenty of sleep now. I always have dark circles under my eyes. I worry that any digestive discomfort could be the start of a flare. Catching a severe stomach virus could land me in the hospital if I were unable to take my meds. I can’t ever forget my meds. Though I try not to let it rule my life, the fear is always there that I will develop colon cancer since IBD patients are more likely to develop it.
Some people plan their day around events, while I still plan mine with restrooms in mind. While a normal person might look for someone they know upon arriving at an event, the first thing I do is locate all the restrooms. I never know for sure when my UC is going to act up. I still miss work on occasion because of a bad UC day, which I define as needing to use the restroom more than three times within an hour.
Pain is ever-present. You know that scale of 1-10 the doctors like to use? Most days, the pain in my left side is between 2-3. I know that doesn’t sound like much, and it’s nothing like the 8-10 I felt when I was admitted to the hospital all those years ago. The thing is, when you spend every day at a 3 without a break, it can start to wear on you the same as if your pain were a 6.
I hope there’s a cure for UC and its sibling, Crohn’s disease in my lifetime. For good measure, I hope to also see cures for cancer, diabetes, SMA, MS, and so many other diseases. Until then, I will continue to fight and live my life as a UC warrior alongside other warriors with more reach than me, like Jake Diekman, pitcher for the Texas Rangers. He started the Gut It Out Foundation to help fund IBD research because of his decades-long battle with UC. I donate to the cause each year.

To learn more about his foundation, visit www.gutitoutfoundation.org.
I am also a member of the Crohn’s and Colitis Foundation, which also raises funds for IBD research. The two organizations, along with others, work together to seek a cure for these horrible diseases.
 To learn more or donate to the cause, visit crohnscolitisfoundation.org.
To learn more or donate to the cause, visit crohnscolitisfoundation.org.
-Brandi Easterling Collins




2 Comments
Cynthia
Did you try diet?
I was diagnosed several years ago- tried every med- all failed! Constant flare! Found specific carbohydrate diet and have been healed drug free since…
caniscareyou
Thank you, Cynthia. I am on a special diet and it helps keep the flares at bay along with my medication.